Abstract
Valproic acid is an anticonvulsant and mood-stabilizing drug used primarily in the treatment of epilepsy and bipolar disorder. Adverse effects of valproic acid are rare, but hepatotoxicity is severe in particular in those younger than 2 years old and polytherapy. During valproic acid treatment, it is difficult for prescribers to predict its individual response. Recent advances in the field of pharmacogenomics have indicated variants of candidate genes that affect valproic acid efficacy and safety. In this review, a large number of candidate genes that influence valproic acid pharmacokinetics and pharmacodynamics are discussed, including metabolic enzymes, drug transporters, neurotransmitters and drug targets. Furthermore, pharmacogenomics is an important tool not only in further understanding of interindividual variability but also to assess the therapeutic potential of such variability in drug individualization and therapeutic optimization.
Similar content being viewed by others
Introduction
Valproic acid (VPA) is a fatty acid having an anticonvulsant property for the treatment of various types of epilepsy and seizures, such as absence, myoclonic, generalized and partial seizures. However, the mechanisms of its therapeutic effect remain to be understood. It can increase the level of γ-aminobutyric acid (GABA) in the brain by inhibiting catabolism of GABA or preventing GABA from reabsorption of glia and nerve endings.1 Valproic acid can also act by restraining neuronal repetitive firing through suppressing voltage-sensitive sodium channel.2 Meanwhile, it is also applied in migraine, bipolar, mood, anxiety, and mental illness widely.3 Recent studies have demonstrated that it acts as histone deacetylase (HDAC) inhibitor to treat cancer, HIV and neurodegenerative disease.4
Although valproic acid has been widely used in various areas, it remains difficult to predict the patient’s individual response to treatment, in terms of efficacy and genetic predisposition. In the clinical, the effective therapeutic plasma level of VPA ranges 50 μg ml−1 to 100 μg ml−1 with a broad recommended dose range. However, plasma concentration may vary greatly among patients taking the same dose of valproic acid.5 With the development of the pharmacogenomics in valproic acid, it is helpful to identify a large amount of candidate genes, such as regulating signaling pathway related transporter, protein, receptor gene mutations, affecting the pharmacokinetic, pharmacodynamic and toxic reaction of VPA.6 In general, a growing number of genes have been demonstrated in influencing its metabolism, efficacy and safety, which partly illustrate interindividual variability among patients taking VPA. Some genetic variants also have been observed to have close relationship with serious side effects, including hepatotoxicity and teratogenicity.6
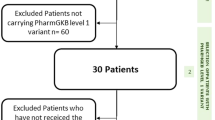
The purpose of this review is to describe the major genetic variants associated with valproic acid metabolism, efficacy and safety. We searched literatures in PubMed using the following key words: valproic acid/VPA/valproate/sodium valproate, polymorphism/SNP/variant. Moreover, additional literatures were identified by cross-references within original or review articles. Meeting or conference abstracts were excluded. A study was included if it conformed to the following criterion: (1) the study regarding the polymorphism and valproic acid; (2) the article types are original or review; (3) can get full text.
Genetic variants that influence the pharmacokinetics of VPA
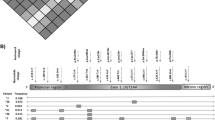
VPA is almost completely metabolized by liver, and only a small percentage of non-metabolized VPA is excreted by urine.7 There are at least three metabolic routes of VPA in human, including the uridine 5′-diphospho-glucuronosyl-transferase (UGT)-mediated pathway, mitochondria β-oxidation pathway (both have been confirmed as major metabolic routes accounting for 50% and 40%, respectively), and CYP-mediated oxidation pathway (a slight route accounting for 10%).8 Currently, a number of studies have confirmed that drug metabolizing enzymes encoded by genes can affect the pharmacokinetic behavior of drugs (Table 1). The following section will examine a large number of candidate genes, associating with the pharmacokinetics of VPA.
Cytochrome P450 enzymes
Numberous studies have demonstrated that specific human cytochrome P450 (CYP) enzymes play a crucial role in the metabolism of VPA. The key CYP-mediated branch of the VPA pathway produces the metabolite of 4-ene-VPA by CYP2C9, CYP2B6, CYP2A6, which may be linked to VPA-induced liver injury.5 Lan Tan et al.9 reported that subjects with one or two CYP2A6*4 alleles variants had a higher VPA mean plasma concentrations than those without. Meanwhile, The subjects with CYP2B6*6 alleles showed higher VPA mean plasma concentrations than those non-*6 alleles. Besides that, subjects with the mutation of CYP2C9*3 also had a higher VPA mean plasma concentrations than those with wild-type genotypes. These mutated alleles in the CYP2A6, CYP2B6, CYP2C9 genes can interpret some of the substantial variability in VPA pharmacokinetics among different subjects. Also, VPA (1 nM) metabolism assay in vitro showed CYP2C9*1 was responsible for the formation of VPA 4-hydroxylation, and VPA 5-hydroxylation activities by 75-80%, while CYP2A6 contributes about 50% of VPA 3-hydroxylation formation; and CYP2A6 and CYP2B6 promote the degree of VPA oxidative metabolism in relation to the catalytic capacity of these enzymes in human hepatic microsomes.10 Another study also confirmed that subjects with CYP2C9*2 and CYP2C9*3 homozygotes reduced the oxidative biotransformation of VPA in liver microsomes compared with subjects with CYP2C9*2/*3 heterozygotes, and catalyzed the formation of 4-ene-VPA, 4-OH-VPA, and 5-OH-VPA.11 Therefore, the knowledge of patients’ CYP2C9 status can contribute to the optimization of VPA dosing and to the avoidance of side effects.12 Nevertheless, the role of CYP2C9 various in attenuation of 4-ene-VPA formation cannot be confirmed in Iranian patients.13 In addition, the study showed that the carriers of CYP2C19*2 allele, an enzyme important for the metabolism of VPA, required higher VPA doses to achieve a VPA concentration of >50 μg ml−1.14 Although CYPs account for a minor part in VPA metabolic pathway, it is important for toxicity in patients with impaired UGTs. Because of the inconsistent results about the influences of CYPs genetic variants on VPA pharmacokinetics, larger cohorts are needed to verify these results and examine the newer candidate genes.
UGT variants
It is well known that glucuronidation conjugation is the predominant route of VPA elimination. Approximately 20–70% of VPA is excreted in the urine as glucuronide conjugates. Currently, a great number of studies on glucuronidation conjugation of valproic acid have focused on these genes, including UGT1A1, UGT1A9, UGT1A4, UGT1A6, UGT1A3, UGT2B7 and UGT2B15.15, 16 A study of recombinant enzymes and human liver microsomes to explore the effect of three non-synonymous polymorphisms (19 T>G, 541A>G and 552A>C) in human UGT1A6 gene. Compared with UGT1A6*1, UGT1A6*2, the variant allele of the above polymorphisms showed 2-fold increased VPA glucuronidation activity.17 However, further work confirmed that the UGT1A6 genotype has no significant effect on serotonin glucuronidation. Similarly, another study of VPA monotherapy and stable epilepsy control in 162 patients with epilepsy revealed that patients with the variant allele of UGT1A6 19 T>G, 541A>G and 552A>C tended to require higher VPA dosages and lower concentration-to-dose ratios (CDRs) than noncarriers.18 This result was also verified in Chinese children with epilepsy.19 Consequently, patients with the UGT1A6 variant genotypes may need to be given a higher VPA maintenance dose compared with those with wild-type genotypes in clinical. However, the effects of these mutated haplotypes and haplotype on VPA dose and CDRs remain to be revealed. Meanwhile, these results should not be overly explained because the sample size is limited, and further work is needed to determine whether UGT1A6 haplotypes contribute to the guidance of the VPA starting doses.
Apart from UGT1A6 variant, UGT2B7 is also discussed widely. A recent study on UGT2B7 −161C>T polymorphism has shown that adjusted plasma VPA concentrations with CC genotype patients are lower than those with CT or TT genotype in pediatric epilepsy patients.20 However, another study did not find a positive association in Chinese epilepsy patients.18 In addition, two studies also confirmed that patients carrying the UGT2B7 802C>T variant allele had significantly higher adjusted VPA concentrations compared with those without variant alleles in Chinese epilepsy patients. But, other studies failed to identify any positive correlation between UGT2B7 802C>T variant and VPA serum concentration.19, 21 Moreover, others studies also found that UGT2B7 genotypes had no influence on the plasma concentration of VPA.22, 23 The limited sample size and age variation may partly explain this inconsistency in different studies. A report showed that VPA clearance values were significantly reduced in elderly patients compared with young people.24 Another study also confirmed that age had a positive correlation with the adjusted serum VPA concentration in pediatric epilepsy patients.23 A study of 242 Chinese epilepsy patients demonstrated that UGT1A3*5 carriers required a higher VPA dose to ensure that the treatment rang was 50–100 μg ml−1.21 However, other reports of the enzyme activities on different UGT1A3 variants appear to be inconsistent with this. Hence, it is arbitrary to infer that UGT1A3 variants affect the plasma concentration of VPA.
Meanwhile, it also has been confirmed that drug transporters play a critical role in pharmacokinetics of VPA, which contributes to the flow of toxins and drugs. The overexpression of efflux drug transporter proteins can also be regulated by the nuclear receptor PXR.25, 26 Among them, the most common drug transporters associated with VPA including P-glycoprotein (P-gp) transporter, Multi-drug-resistance protein transporter, which have pharmacogenetic relevance. P-gp is an energy-dependent efflux pump that excludes several antiepileptic drugs (AEDs), which is the product of the ATP-binding cassette subfamily b member 1 (ABCB1), also known as the multi-drug resistance 1 (MDR1) gene.27, 28 The current researches mainly focused on the study of genetic polymorphisms of ABCB1 C3435T, G2677T/A and C1236T polymorphisms. A study showed that the ABCB1 C3435T polymorphism is significantly relevant to drug resistance in patients with epilepsy, which is defined as failure of two (or more) adequate trials of tolerated, appropriately chosen, and appropriately used antiepileptic drug regimens (mono-or polytherapies) to achieve sustained seizure freedom.29 And patients with CC genotype at ABCB1 3435 were more likely to be resistant compared with the TT genotype.30 A meta-analysis result also indicates that ABCB1 G2677T/A polymorphism may increase the risk of drug resistance epilepsy in Asians.31 However, other studies have failed to find a significant correlations with these polymorphism in pharmacokinetics of VPA.32, 33, 34 Many factors may be attributed to the inconsistency and poor repeatability of results among all types of studies, including insufficient sample size, non-consensus the definition of intractability and genetic heterogeneity among studies. Apart from ABCB1 transporters, the role of the other efflux transporter ABCC2 (multi-drug-resistance protein 2, MRP2) has also attracted more and more attentions. It has been investigated that ABCC2 gene may determine individual sensitivity of VPA to central nervous system adverse drug reactions (ADRs) by limiting the presence of antiepileptic drugs into the brain.35
Genetic polymorphism may be a critical source of interindividual differences in the pharmacokinetics of VPA. The dosage optimization has a significant role in the treatment of epilepsy, thus exploring genetic factors that influence the pharmacokinetics of VPA may help to improve individualized therapies so that epilepsy patients receive more effective treatment. Although VPA is substrate of a variety of UGT isozymes and it has been found that many single nucleotide polymorphisms in genes are associated with VPA metabolism, and the current studies have not yet yielded definite judgments about their effects on VPA glucuronation or clinical significance. Hence, in order to determine the detailed enzymatic nature of the various UGTs and CYPs variants, much work remains to be done. Future studies should place emphasis on clinical studies of these genes to elucidate the effect of polymorphisms on clinical outcomes.
Genetic variants that influence the pharmacodynamics of VPA
VPA displays its pharmacodynamics effects in three pathways, including acting on γ-aminobutyric acid (GABA) levels, blocking ion channels, and also acting as histone deacetylase (HDAC) inhibitor.6 In the brain, VPA changes the activity of the neurotransmitter GABA by inhibiting GABA degradation, inhibiting GABA transaminase (ABAT), increasing its synthesis, and reducing conversion.3, 36In vitro researches have exhibited that VPA inhibits GABA transaminase (ABAT), succinate semialdehyde dehydrogenase (ALDH5A1), and α-ketoglutarate dehydrogenase (OGDH) to increase GABA levels in the brain.2, 6 A study result on 201 epileptic patients in Chinese also demonstrated that ABAT and ALDH5A1 may play important roles in the pharmacological mechanism of VPA.37, 38
Besides acting on GABA levels in the brain, VPA may reduce excitability by blocking various ion channels, including voltage-gated sodium channel (SCN gene family), potassium channel, and calcium channel.2, 39 However, whether the conductance of potassium channels will affect VPA response is still unknown. Previous studies also found that the polymorphisms of SCN2A rs2304016 was significantly associated with the efficacy of VPA.37, 40 However, the results of meta-analysis demonstrated that SCN1A, SCN2A and SCN3A gene polymorphisms had no significant effects on VPA efficacy.40, 41 Meanwhile, as another important ion channel, calcium channel not merely participate in epileptogenesis but as a common antiepileptic drug target. However, the literature revealed no significant correlation between the CACNA1A, CACNA1C, CACNA1H and drug efficacy in Chinese population.42
Recently, VPA has been used as an HDAC inhibitor, which plays an important role in gene transcription by suppressing histone deacetylation and influences several crucial approaches, including DNA repair, apoptosis, cell cycle control, and differentiation.43, 44 VPA specifically targets HDAC9 and HDAC11, which are closely related to neuronal function and could partly illuminate the role of VPA in neuropathology.3 VPA-induced overexpression of specific deacetylases in AML and increased the response of antineoplastic therapies by killing tumor cells.45 In addition, VPA could stimulate the generation of less mature cell by targeting HDAC2; VPA could only enhance a single aspect of osteoblast differentiation, and thus produce selective effects by RNA interference.46
Because of the majority of current studies focusing on the pharmacokinetic genes of VPA, the pharmacodynamics genes of VPA were ignored. Moreover, many of previous study results have not been replicated in other independent population. So genetic variants that influence the pharmacodynamics of VPA is largely unknown.
Genetic variants that influence the VPA toxicity
Although VPA is one of the most commonly used AEDs in the world, it may be limited due to lack of efficacy, or serious ADR. Severe ADRs include liver damage, mitochondria toxicity, teratogenicity, hyperammonemia encephalopathy and other adverse events.47 A study on freshly isolated rat hepatocytes has indicated that VPA-induced oxidative stress and mitochondria dysfunction precedes hepatotoxicity in rat.48 In addition, VPA also induced hepatotoxicity by involving lysosomal membrane leakage as well as reactive oxygen species (ROS) formation which as a result of metabolic activation by CYP2E1.49 CYP2E1 is an effective enzyme for ROS production and is one of the most powerful inducers of oxidative stress in cells.50 VPA-induced ROS formation was protected by inhibitors of CYP2E1 (1-phenylimidazole, and 4-methylpyrazole). Genetic and environmental factors could affect the patients susceptibility to adverse reactions of VPA (Table 2). Moreover, the FDA-approved VPA drug labels indicated contraindications in patients with urea cycle disorders (UCDs), who often experience fatal hyperammonemia encephalopathy after initiation of treatment. It has been confirmed that five key enzymes take part in the urea cycle, including carbamoyl phosphate synthetase 1 (CPS1), ornithine transcarbamoylase (OTC), argininosuccinate synthase (ASS1), argininosuccinate lyase (ASL), and arginase 1 (ARG1).51 Another N-acetylglutamate synthase (NAGS) expressed in the mitochondrion, is also important for the function of the urea cycle because it provides the necessary mutant activator N-acetylglutamic acid (NAG). A study in rat liver mitochondria demonstrated that the metabolite valproyl-CoA inhibits NAGS activity, resulting in accumulation of ammonia.52 CPS1 is the first rate-limiting enzyme in the urea cycle, which accelerates the transformation of ammonium into carbamoyl phosphate in the liver. CPS1 function dysregulation could be resulted from genetic variation or epigenetic regulation in hepatocellular carcinoma.53 Therefore, it is conceivable that the lack of CPS1 or a decrease in activity may be largely related to VPA-induced hyperammonemia. CPS1 4217C>A polymorphism is an amino acid conversion from threonine to asparagine, which is correlated with a poor CPS1 activity. A study in Japanese epileptic patients undergoing VPA co-administered with other anticonvulsants demonstrated that CPS1 4217C>A polymorphism was a risk factor for hyperammonemia.54 This result was also verified in Caucasian epileptic patients.55 However, a study in Japanese population found that this polymorphism may not be associated with the evolution of hyperammonemia during the treatment of VPA.56 This inconsistency can be caused by the number of co-administered antiepileptic drugs and the small sample size. In addition, ammonia is also consumed by glutamine synthetase in the urea cycle, which is encoded by glutamine synthetase gene (GLUL). A study found that GLUL rs107997771 polymorphism was a newfound risk factor for the evolution of serious hyperammonemia during the treatment of VPA.57 However, the results have not been further verified and repeated in other studies. And the incidence of abnormal increase in serum ammonia during VPA treatment was reported to have increased from 16.2% to 52.3%,58 while the potential mechanisms for the elevated plasma ammonia level remains unclear. So it is necessary to conduct further investigations to explore the association between CPS1 polymorphisms and the development of hyperammonemia.
In addition, VPA is also forbidden in patients with polymerase γ gene (POLG) variations. POLG is defined as mitochondria DNA polymerase that is associated with various disorders such as Alpers Huttenlocher Syndrome (AHS), which is associated with an increased risk of fatal VPA liver toxicity. Approximately one-third of AHS patients developed hepatic failure within 3 months after VPA treatment. Common functional genetic variants of POLG are present in up to 0.5% of the population.59 It has been confirmed that genetic mutations in POLG was significantly related to VPA-induced hepatotoxicity.60, 61 VPA treatment resulted in a significant overexpression of POLG and triggered increasing of mitochondria biogenesis by changing the expression of several mitochondria genes.62 The heterozygous p.Q1236H and p.E1143G mutations in POLG1 gene were associated with VPA-induced hepatic failure.60, 63 Therefore, POLG mutation testing should be carried out in patients with suspected mitochondria disease before VPA treatment, and should be avoided in these patients with VPA treatment. Filtering functional POLG markers will minimize the risk of hepatic failure in patients with VPA-based therapy. So further work is needed to identify the relationship between more genetic variation of POLG and liver injury during VPA therapy.
Additional new pharmacogenomics candidates for VPA-induced liver injury included glutathione S-transferases (GSTs), catalyzing the inactivation of various endogenous substances by oxidative stress in the liver. The study demonstrated a significant increase in γ-glutamyltransferase (GGT) levels in patients with GSTM1- genotype and GSTM1-/GSTT1- genotypes in VPA-treated patients.64 Elevated serum GGT activity in VPA-treated patients may be caused by the elimination of liver GSH and it was also presented as an early maker of oxidative stress. However, the clinical association between the GGT levels and the GST polymorphism to VPA therapy remained unknown. It was insufficient to prove whether the increase in GGT levels resulted from VPA-induced liver toxicity. Also, the functional polymorphism in SOD2 gene was demonstrated to be associated with the VPA-induced elevation of serum aminotransferases.65 It was reported that about one-third of patients with VPA monotherapy occurred the liver adverse reactions, and the severity of liver toxicity can be from reversible liver dysfunction to irreversible hepatic failure. It would be interesting to investigate the mechanism of VPA-induced liver injury in the future. Apart from hepatotoxicity, VPA also induced teratogenicity by down-regulated genes IGF2R, RGS4, COL6A3, EDNRB and KLF6, which is relevantly related to the prevalence of neural tubular defect (NTD) in chicken embryo model.66 It is also found that patients with BsmI polymorphism, a useful genetic maker of bone mineral density and the risk of osteoporosis, had significantly higher total levels of cholesterol, triglycerides, high density lipoprotein cholesterol (HDL-C) and low density lipoprotein cholesterol (LDL-C), which increased the risk of vascular risk factors.67 The 116C/G (rs226957) variant in the promoter region of XBP1 is associated with bipolar disorders. Valproate actives transcription factor 6, in the gene upstream of XBP1, increasing treatment response with the G allele in bipolar disorder.68 In addition, the newly found candidates genes associated with VPA included LEPR and ANKK1, which may be valuable in predicting VPA-induced weight gain.69 VPA was also found to downgrade URG4/URGCP and CCND1 gene expression to suppress the proliferation of SHSY5Y neuroblastoma cell.70
Conclusion
Pharmacogenomics is amid at exploring the individual differences in their response to drug therapy and the mechanism of pathogenesis. Different individual has a different genetic makeup, which is related to the risk of evolving diseases and variable drug response. Therefore, the understanding of genetic variations in interindividual drug response behaviors have become an urgent affairs. Our study aimed at discussing the pharmacogenomics of VPA, which has been used in various areas widely, including various epileptic seizures, migraine, bipolar disorder, anxiety, psychiatric disorders, and cancer, HIV, as well as neurodegenerative disease. However, with a broad recommended dose range and a wide effective therapeutic plasma level (50–100 μg ml−1), the does requirements for VPA are highly variable (10-fold differences in mean dose in adults).5 The pharmacological treatment of epilepsy has been empirical and often based on trial and error, such as increasing or decreasing the doses of AEDs, switching or adding another AEDs.71 Although the plasma concentrations and doses of VPA are highly correlated, the concentrations do not correlate well with the therapeutic effects of the VPA. Therefore, a study developed an equation regarding the relationship between the serum VPA concentrations and the seizure control by developing a population-based pharmacokinetic (PK)-pharmacodynamic (PD) model. The model showed that age, seizure locus, SCN1A rs3812718 polymorphism and co-administration of carbamazepine, clonazepam, phenytoin or topiramate were associated with an over 50% reduction in the seizure frequency.72 It may be useful to determine the recommended therapeutic concentration of AEDs for each patient, and may contribute to the further development of individualized treatment. Therefore, more PK-PD models should be performed among a larger patient population, and more genetic factors should also be considered. Moreover, the above studies demonstrated that multiple genetic effects were involved in VPA treatment and safety. Over the past few decades, a large number of possible candidate genes have been found to be associated with VPA genetic behaviors. These surveys presented new insights into the individualized use of VPA. It seems plausible that VPA played a role through several different mechanisms including metabolic enzymes, different neurotransmitters, and drug targets. But very few studies have identified genomic variants that influence VPA dosage, VPA-induced toxicity and treatment effect. Although VPA therapy is relatively safe, it still has many ADRs, including liver damage, mitochondria toxicity, teratogenicity, hyperammonemia encephalopathy and other adverse events. Rare polymorphism or ethnic-related mutations may be related to toxic reactions and idiosyncratic adverse effects, and genotyping of patients presenting toxicity signs may lead to answers regarding the underlying mechanisms and possible prevention of such reactions. Thus further studies should be performed to determine the genetic variations in interindividual drug response behaviors and drug safety. Complementary metabolomics studies may also aid in profiling patients at risk for ADRs. At present, the majority of studies have concentrated on the polymorphisms of CYP and UGT candidate genes, whereas mitochondria genes that may affect VPA metabolism directly or indirectly are yet to be explored. The catalysis of VPA metabolism by CYP enzymes could accelerate the formation of metabolic products such as 4-ene-VPA, thereby increasing the risk of mitochondria stress and liver toxicity.10, 13 Many candidate genes have been thought to induce VPA liver injury, including CPS1 and POLG mutation. However, inconsistent results restrict the credibility of their correlation of pharmacogenomics due to insufficient sample size and the poor repeatability. Thus the current findings need to be verified among large cohorts, and pediatric cohorts in particular, which includes patients from other ethnic groups, and examining the action of new candidate genes and mutations in VPA therapy. Further research should also focus on clinical studies of genotype-phenotype correlations of these genes to clarify the impact of various polymorphisms on clinical level. Meanwhile, the advantages of pharmacogenomics researches far outweigh the single identification of genes that could play an important role in personalized medicine in the future.
References
Bialer, M. Why are antiepileptic drugs used for nonepileptic conditions? Epilepsia 53, 26–33 (2012).
Johannessen, C. U. & Johannessen, S. I. Valproate: past, present, and future. CNS Drug Rev. 9, 199–216 (2003).
Chateauvieux, S., Morceau, F., Dicato, M. & Diederich, M. Molecular and therapeutic potential and toxicity of valproic acid. J. Biomed. Biotechnol. 2010, pii:479364 (2010).
Phiel, C. J., Zhang, F., Huang, E. Y., Guenther, M. G., Lazar, M. A. & Klein, P. S. Histone deacetylase is a direct target of valproic acid, a potent anticonvulsant, mood stabilizer, and teratogen. J. Biol. Chem. 276, 36734–36741 (2001).
Ferraro, T. N. & Buono, R. J. The relationship between the pharmacology of antiepileptic drugs and human gene variation: an overview. Epilepsy Behav. 7, 18–36 (2005).
Ghodke-Puranik, Y., Thorn, C. F., Lamba, J. K., Leeder, J. S., Song, W., Birnbaum, A. K. et al. Valproic acid pathway: pharmacokinetics and pharmacodynamics. Pharmacogenet. Genomics 23, 236–241 (2013).
Dickinson, R. G., Hooper, W. D., Dunstan, P. R. & Eadie, M. J. Urinary excretion of valproate and some metabolites in chronically treated patients. Ther. Drug Monit. 11, 127–133 (1989).
DeVane, C. L. Pharmacokinetics, drug interactions, and tolerability of valproate. Psychopharmacol. Bull. 37, 25–42 (2003).
Tan, L., Yu, J., Sun, Y., Ou, J., Song, J. & Yu, Y. The influence of cytochrome oxidase CYP2A6, CYP2B6, and CYP2C9 polymorphisms on the plasma concentrations of valproic acid in epileptic patients. Clin. Neurol. Neurosurg. 112, 320–323 (2010).
Kiang, T. K. L., Ho, P. C., Anari, M. R., Tong, V., Abbott, F. S. & Chang, T. K. H. Contribution of CYP2C9, CYP2A6, and CYP2B6 to valproic acid metabolism in hepatic microsomes from individuals with the CYP2C9*1/*1 genotype. Toxicol. Sci. 94, 261–271 (2006).
Ho, P. C., Abbott, F. S., Zanger, U. M. & Chang, T. K. Influence of CYP2C9 genotypes on the formation of a hepatotoxic metabolite of valproic acid in human liver microsomes. Pharmacogenomics J. 3, 335–342 (2003).
Budi, T., Toth, K., Nagy, A., Szever, Z., Kiss, A., Temesvari, M. et al. Clinical significance of CYP2C9-status guided valproic acid therapy in children. Epilepsia 56, 849–855 (2015).
Amini-Shirazi, N., Ghahremani, M. H., Ahmadkhaniha, R., Mandegary, A., Dadgar, A., Abdollahi, M. et al. Influence of CYP2C9 polymorphism on metabolism of valproate and its hepatotoxin metabolite in Iranian patients. Toxicol. Mech. Methods 20, 452–457 (2010).
Voso, M. T., Santini, V., Finelli, C., Musto, P., Pogliani, E., Angelucci, E. et al. Valproic acid at therapeutic plasma levels may increase 5-azacytidine efficacy in higher risk myelodysplastic syndromes. Clin. Cancer. Res. 15, 5002–5007 (2009).
Chatzistefanidis, D., Georgiou, I., Kyritsis, A. P. & Markoula, S. Functional impact and prevalence of polymorphisms involved in the hepatic glucuronidation of valproic acid. Pharmacogenomics 13, 1055–1071 (2012).
Zhang, L., Chu, X., Wang, H., Xie, H., Guo, C., Cao, L. et al. Dysregulations of UDP-glucuronosyltransferases in rats with valproic acid and high fat diet induced fatty liver. Eur. J. Pharmacol. 721, 277–285 (2013).
Krishnaswamy, S., Hao, Q., Al-Rohaimi, A., Hesse, L. M., von, Moltke, L. L., Greenblatt, D. J. et al. UDP glucuronosyltransferase (UGT) 1A6 pharmacogenetics: II. Functional impact of the three most common nonsynonymous UGT1A6 polymorphisms (S7A, T181A, and R184S). J. Pharmacol. Exp. Ther. 313, 1340–1346 (2005).
Hung, C. C., Ho, J. L., Chang, W. L., Tai, J. J., Hsieh, T. J., Hsieh, Y. W. et al. Association of genetic variants in six candidate genes with valproic acid therapy optimization. Pharmacogenomics 12, 1107–1117 (2011).
Guo, Y., Hu, C., He, X., Qiu, F. & Zhao, L. Effects of UGT1A6, UGT2B7, and CYP2C9 genotypes on plasma concentrations of valproic acid in Chinese children with epilepsy. Drug Metab. Pharmacokinet. 27, 536–542 (2012).
Inoue, K., Suzuki, E., Yazawa, R., Yamamoto, Y., Takahashi, Y., Imai, K. et al. Influence of uridine diphosphate glucuronosyltransferase 2B7 -161C>T polymorphism on the concentration of valproic acid in pediatric epilepsy patients. Ther. Drug Monit. 36, 406–409 (2014).
Chu, X. M., Zhang, L. F., Wang, G. J., Zhang, S. N., Zhou, J. H. & Hao, H. P. Influence of UDP-glucuronosyltransferase polymorphisms on valproic acid pharmacokinetics in Chinese epilepsy patients. Eur. J. Clin. Pharmacol. 68, 1395–1401 (2012).
Sun, Y. X., Zhuo, W. Y., Lin, H., Peng, Z. K., Wang, H. M., Huang, H. W. et al. The influence of UGT2B7 genotype on valproic acid pharmacokinetics in Chinese epilepsy patients. Epilepsy Res. 114, 78–80 (2015).
Wang, Q., Zhao, L., Liang, M., Dong, Y., Yun, W., Qiu, F. et al. Effects of UGT2B7 genetic polymorphisms on serum concentrations of valproic acid in Chinese children with epilepsy comedicated with lamotrigine. Ther. Drug Monit. 38, 343–349 (2016).
Fattore, C., Messina, S., Battino, D., Croci, D., Mamoli, D. & Perucca, E. The influence of old age and enzyme inducing comedication on the pharmacokinetics of valproic acid at steady-state: a case-matched evaluation based on therapeutic drug monitoring data. Epilepsy Res. 70, 153–160 (2006).
Stepien, K. M., Tomaszewski, M., Tomaszewska, J. & Czuczwar, S. J. The multidrug trans- porter P-glycoprotein in pharmacoresistance to antiepileptic drugs. Pharmacol. Rep. 64, 1011–1019 (2012).
Kumari, R., Lakhan, R., Garg, R. K., Kalita, J., Misra, U. K. & Mittal, B. Pharmacogenomic association study on the role of drug metabolizing, drug transporters and drug target gene polymorphisms in drug-resistant epilepsy in a north Indian population. Indian. J. Hum. Genet. 17, S32–S40 (2011).
Sisodiya, S. M. Mechanisms of antiepileptic drug resistance. Curr. Opin. Neurol. 16, 197–201 (2003).
Hung, C. C., Chen, C. C., Lin, C. J. & Liou, H. H. Functional evaluation of polymorphisms in the human ABCB1 gene and the impact on clinical responses of antiepileptic drugs. Pharmacogenet. Genomics 18, 390–402 (2008).
Kwan, P., Arzimanoglou, A., Berg, A. T., Brodie, M. J., Allen Hauser, W., Mathern, G. et al. Definition of drug resistantepilepsy: consensus proposal by the ad hoc Task Force of the ILAE Commissionon Therapeutic Strategies. Epilepsia 51, 1069–1077 (2010).
Siddiqui, A., Kerb, R., Weale, M. E., Brinkmann, U., Smith, A., Goldstein, D. B. et al. Association of multidrug resistance in epilepsy with a polymorphism in the drug-transporter gene ABCB1. N. Engl. J. Med. 348, 1442–1448 (2003).
Yu, L., Liao, W., Yi, Y. & Qiu, G. ABCB1 G2677T/A polymorphism is associated with the risk of drug-resistant epilepsy in Asians. Epilepsy Res. 115, 100–108 (2015).
Haerian, B. S., Lim, K. S., Mohamed, E. H., Tan, H. J., Tan, C. T., Raymond, A. A. et al. Lack of association of ABCB1 and PXR polymorphisms with response to treatment in epilepsy. Seizure 20, 387–394 (2011).
Haerian, B. S., Lim, K. S., Tan, H. J., Mohamed, E. H., Tan, C. T., Raymond, A. A. et al. Association between ABCB1 polymorphism and response to sodium valproate treatment in Malaysian epilepsy patients. Epileptic Disord. 13, 65–75 (2011).
Turgut, G., Kurt, E., Sengul, C., Alatas, G., Kursunluoglu, R., Oral, T. et al. Association of MDR1 C3435T polymorphism with bipolar disorder in patients treated with valproic acid. Mol. Biol. Rep. 36, 495–499 (2009).
Yi, J. H., Cho, Y., Kim, W., Lee, M. G. & Lee, J. H. Genetic variations of ABCC2 gene associated with adverse drug reactions to valproic acid in Korean epileptic patients. Genomics Inform. 11, 254–262 (2013).
Mesdjian, E., Ciesielski, L., Valli, M., Bruguerolle, B., Jadot, G., Bouyard, P. et al. Sodium valproate: kinetic profile and effects on GABA levels in various brain areas of the rat. Prog. Neuropsychopharmacol. Biol. Psychiatry 6, 223–233 (1982).
Li, X., Zhang, J., Wu, X., Yan, H., Zhang, Y., He, R. H. et al. Polymorphisms of ABAT, SCN2A and ALDH5A1 may affect valproic acid responses in the treatment of epilepsy in Chinese. Pharmacogenomics 17, 2007–2014 (2016).
Shinka, T., Ohfu, M., Hirose, S. & Kuhara, T. Effect of valproic acid on the urinary metabolic profile of a patient with succinic semialdehyde dehydrogenase deficiency. J. Chromatogr. B Analyt. Technol. Biomed. Life Sci. 792, 99–106 (2003).
VanDongen, A. M., VanErp, M. G. & Voskuyl, R. A. Valproate reduces excitability by blockage of sodium and potassium conductance. Epilepsia 27, 177–182 (1986).
Haerian, B. S., Baum, L., Kwan, P., Tan, H. J., Raymond, A. A. & Mohamed, Z. SCN1A,SCN2A andSCN3A gene polymorphisms and responsiveness to antiepileptic drugs: a multicenter cohort study and meta-analysis. Pharmacogenomics 14, 1153–1166 (2013).
Haerian, B. S., Baum, L., Tan, H. J., Kwan, P., Raymond, A. A., Saruwatari, J. et al. SCN1A IVS5N+5 polymorphism and response to sodium valproate: a multicenter study. Pharmacogenomics 13, 1477–1485 (2012).
Lv, N., Qu, J., Long, H., Zhou, L., Cao, Y., Long, L. et al. Association study between polymorphisms in the CACNA1A, CACNA1C, and CACNA1H genes and drug-resistant epilepsy in the Chinese Han population. Seizure 30, 64–69 (2015).
Gottlicher, M., Minucci, S., Zhu, P., Kramer, O. H., Schimpf, A., Giavara, S. et al. Valproic acid defines a novel class of HDAC inhibitors inducing differentiation of transformed cells. EMBO J. 20, 6969–6978 (2001).
Chavez-Blanco, A., Perez-Plasencia, C., Perez-Cardenas, E., Carrasco-Legleu, C., Rangel-Lopez, E., Segura-Pacheco, B. et al. Antineoplastic effects of the DNA methylation inhibitor hydralazine and the histone deacetylase inhibitor valproic acid in cancer cell lines. Cancer Cell Int. 6, 2 (2006).
Bradbury, C. A., Khanim, F. L., Hayden, R., Bunce, C. M., White, D. A., Drayson, M. T. et al. Histone deacetylases in acute myeloid leukaemia show a distinctive pattern of expression that changes selectively in response to deacetylase inhibitors. Leukemia 19, 1751–1759 (2005).
Paino, F., La, Noce, M., Tirino, V., Naddeo, P., Desiderio, V., Pirozzi, G. et al. Histone deacetylase inhibition with valproic acid downregulates osteocalcin gene expression in human dental pulp stem cells and osteoblasts: evidence for HDAC2 involvement. Stem Cells 32, 279–289 (2014).
Nanau, R. M. & Neuman, M. G. Adverse drug reactions induced by valproic acid. Clin. Biochem. 46, 1323–1338 (2013).
Tong, V. Valproic acid II: effects on oxidative stress, mitochondria membrane potential, and cytotoxicity in glutathione-depleted rat hepatocytes. Toxicol. Sci. 86, 436–443 (2005).
Pourahmad, J., Eskandari, M. R., Kaghazi, A., Shaki, F., Shahraki, J. & Fard, J. K. A new approach on valproic acid induced hepatotoxicity: involvement of lysosomal membrane leakiness and cellular proteolysis. Toxicol. In Vitro 26, 545–551 (2012).
Hassan, H. M., Guo, H., Yousef, B. A., Guerram, M., Hamdi, A. M., Zhang, L. et al. Role of inflammatory and oxidative stress, cytochrome P450 2E1, and bile acid disturbance in rat liver injury induced by isoniazid and lipopolysaccharide cotreatment. Antimicrob. Agents Chemother. 60, 5285–5293 (2016).
Mitchell, S., Ellingson, C., Coyne, T., Hall, L., Neill, M., Christian, N. et al. Genetic variation in the urea cycle: a model resource for investigating key candidate genes for common diseases. Hum. Mutat. 30, 56–60 (2009).
Aires, C. C., van, Cruchten, A., Ijlst, L., de, Almeida, I. T., Duran, M., Wanders, R. J. et al. New insights on the mechanisms of valproate-induced hyperammonemia: inhibition of hepatic N-acetylglutamate synthase activity by valproyl-CoA. J. Hepatol. 55, 426–434 (2011).
Liu, H., Dong, H., Robertson, K. & Liu, C. DNA methylation suppresses expression of the urea cycle enzyme carbamoyl phosphate synthetase 1 (CPS1) in human hepatocellular carcinoma. Am. J. Pathol. 178, 652–661 (2011).
Yagi, M., Nakamura, T., Okizuka, Y., Oyazato, Y., Kawasaki, Y., Tsuneishi, S. et al. Effect of CPS1 4217C>A genotype on valproic-acid-induced hyperammonemia. Pediatr. Int. 52, 744–748 (2010).
Janicki, P. K., Bezinover, D., Postula, M., Thompson, R. S., Acharya, J., Acharya, V. et al. Increased occurrence of valproic acid-induced hyperammonemia in carriers of T1405N polymorphism in carbamoyl phosphate synthetase 1 gene. ISRN Neurol 2013, 1–4 (2013).
Inoue, K., Suzuki, E., Takahashi, T., Yamamoto, Y., Yazawa, R., Takahashi, Y. et al. 4217C>A polymorphism in carbamoyl-phosphate synthase 1 gene may not associate with hyperammonemia development during valproic acid-based therapy. Epilepsy Res. 108, 1046–1051 (2014).
Inoue, K., Takahashi, T., Yamamoto, Y., Suzuki, E., Takahashi, K., Imai, K. et al. Influence of glutamine synthetase gene polymorphisms on the development of hyperammonemia during valproic acid-based therapy. Seizure 33, 76–80 (2015).
Verrotti, A., Trotta, D., Morgese, G. & Chiarelli, F. Valproate-induced hyperammonemic encephalopathy. Metab. Brain. Dis. 17, 367–373 (2002).
Hudson, G. Mitochondria DNA polymerase-γ and human disease. Hum. Mol. Genet. 15, R244–R252 (2006).
Stewart, J. D., Horvath, R., Baruffini, E., Ferrero, L., Bulst, S., Watkins, P. B. et al. Polymerase γ Gene POLG determines the risk of sodium valproate-induced liver toxicity. Hepatology 52, 1791–1796 (2010).
Saneto, R. P., Lee, I. C., Koenig, M. K., Bao, X., Weng, S. W., Naviaux, R. K. et al. POLG DNA testing as an emerging standard of care before instituting valproic acid therapy for pediatric seizure disorders. Seizure 19, 140–146 (2010).
Sitarz, K. S., Elliott, H. R., Karaman, B. S., Relton, C., Chinnery, P. F. & Horvath, R. Valproic acid triggers increased mitochondria biogenesis in POLG-deficient fibroblasts. Mol. Genet. Metab. 112, 57–63 (2014).
Hynynen, J., Komulainen, T., Tukiainen, E., Nordin, A., Arola, J., Kalviainen, R. et al. Acute liver failure after valproate exposure in patients with POLG1 mutations and the prognosis after liver transplantation. Liver Transpl. 20, 1402–1412 (2014).
Fukushima, Y., Seo, T., Hashimoto, N., Higa, Y., Ishitsu, T. & Nakagawa, K. Glutathione-S-transferase (GST) M1 null genotype and combined GSTM1 and GSTT1 null genotypes are risk factors for increased serum γ-glutamyltransferase in valproic acid-treated patients. Clin. Chim. Acta 389, 98–102 (2008).
Saruwatari, J., Deguchi, M., Yoshimori, Y., Noai, M., Yoshida, S., Ogusu, N. et al. Superoxide dismutase 2 Val16Ala polymorphism is a risk factor for the valproic acid-related elevation of serum aminotransferases. Epilepsy Res. 99, 183–186 (2012).
Hsieh, C. L., Chen, K. C., Ding, C. Y., Tsai, W. J., Wu, J. F. & Peng, C. C. Valproic acid substantially downregulated genes folr1, IGF2R, RGS2, COL6A3, EDNRB, KLF6, and pax-3, N-acetylcysteine alleviated most of the induced gene alterations in chicken embryo model. Rom. J. Morphol. Embryol. 54, 993–1004 (2013).
Phabphal, K. & Geater, A. The association between BsmI polymorphism and risk factors for atherosclerosis in patients with epilepsy taking valproate. Seizure 22, 692–697 (2013).
Kim, B., Kim, C. Y., Lee, M. J. & Joo, Y. H. Preliminary evidence on the association between XBP1-116C/G polymorphism and response to prophylactic treatment with valproate in bipolar disorders. Psychiat. Res. 168, 209–212 (2009).
Li, H., Wang, X., Zhou, Y., Ni, G., Su, Q., Chen, Z. et al. Association of LEPR and ANKK1 gene polymorphisms with weight gain in epilepsy patients receiving valproic acid. Int. J. Neuropsychopharmacol 18, 1–7 (2015).
Dodurga, Y., Gundogdu, G., Tekin, V., Koc, T., Satiroglu-Tufan, N. L., Bagci, G. et al. Valproic acid inhibits the proliferation of SHSY5Y neuroblastoma cancer cells by downregulating URG4/URGCP and CCND1 gene expression. Mol. Biol. Rep. 41, 4595–4599 (2014).
Schmidt, D. & Schachter, S. C. Drug treatment of epilepsy in adults. BMJ 28, 348 g254 (2014).
Nakashima, H., Oniki, K., Nishimura, M., Ogusu, N., Shimomasuda, M. & Ono, T. Determination of the optimal concentration of valproic acid in patients with epilepsy: a population pharmacokinetic-pharmacodynamic analysis. PLoS ONE 10, e0141266 (2015).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Zhu, MM., Li, HL., Shi, LH. et al. The pharmacogenomics of valproic acid. J Hum Genet 62, 1009–1014 (2017). https://doi.org/10.1038/jhg.2017.91
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/jhg.2017.91
This article is cited by
-
In silico investigation of potential phytoconstituents against ligand- and voltage-gated ion channels as antiepileptic agents
3 Biotech (2024)
-
Acute pancreatitis during valproic acid administration in a patient with vascular dementia, epileptic seizures, and psychiatric symptoms: a case report
Journal of Medical Case Reports (2023)
-
VPA mediates bidirectional regulation of cell cycle progression through the PPP2R2A-Chk1 signaling axis in response to HU
Cell Death & Disease (2023)
-
The Effect of Berberine Follow by Blue Light Irradiation and Valproic Acid on the Growth Inhibition of MDA-MB-231 Breast Cancer Cells
Applied Biochemistry and Biotechnology (2023)
-
Valproic acid radiosensitizes anaplastic thyroid cells through a decrease of the DNA damage repair capacity
Journal of Endocrinological Investigation (2023)